The 12 Lead ECG
Interpretation that matters!
Introduction to 12-Lead ECG Interpretation for Student Paramedics
A 12-lead ECG is one of the most powerful assessment tools available to paramedics and ambulance clinicians. Unlike rhythm strips, which show the heart’s electrical activity over time, a 12-lead ECG provides multiple views of the heart from different angles, allowing clinicians to assess rhythm, conduction, and signs of myocardial ischaemia or infarction.
For student paramedics, 12-lead ECGs often feel overwhelming, not because they are inherently difficult, but because they are frequently introduced before the foundations are secure. This page provides a structured introduction to 12-lead ECGs, focusing on what they show, how to approach them as a whole, and when they matter in pre-hospital care.
12 Lead ECG Placement
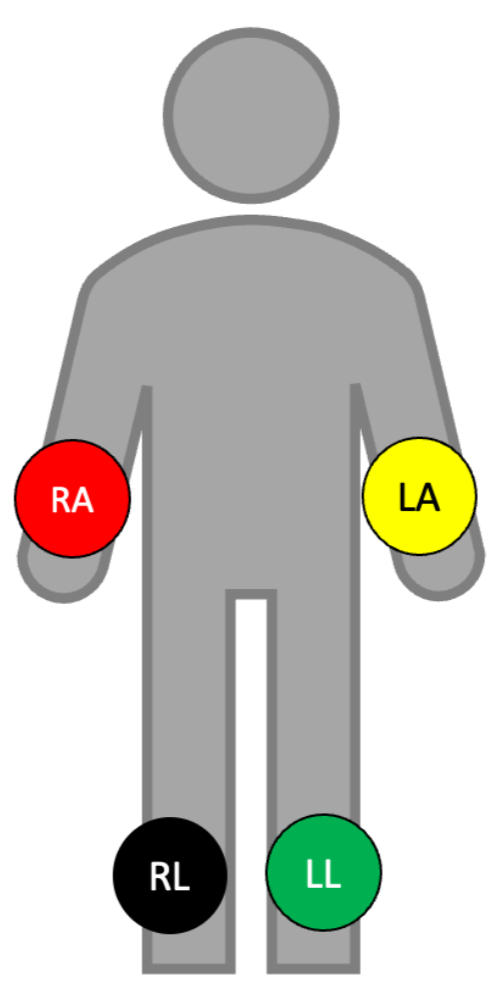
Limb Lead Placement
The limb leads are four stickers that attach to the patient’s wrists and ankles, or if their limbs are shaking due to hypothermia, Parkinson's disease etc then you can place them on the shoulders and hips.
Red: Right upper limb
Yellow: Left upper limb
Green: Left lower limb
Black: Right lower limb
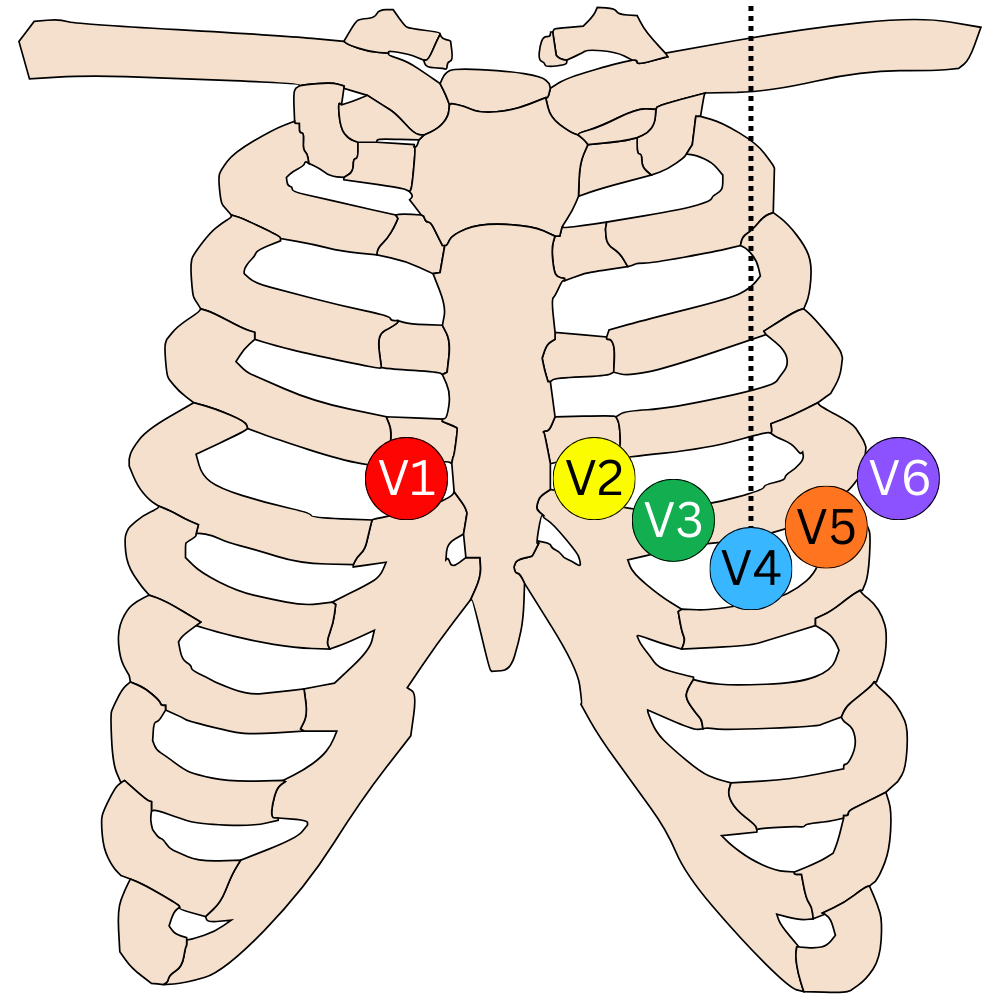
Chest Lead Placement
V1: 4th intercostal space, right of sternal border.
V2: 4th intercostal space, left of sternal border.
V3: In between V2 and V4.
V4: 5th intercostal space, mid-clavicular line.
V5: 5th intercostal space, anterior axillary line.
V6: 5th intercostal space, mid axillary line.
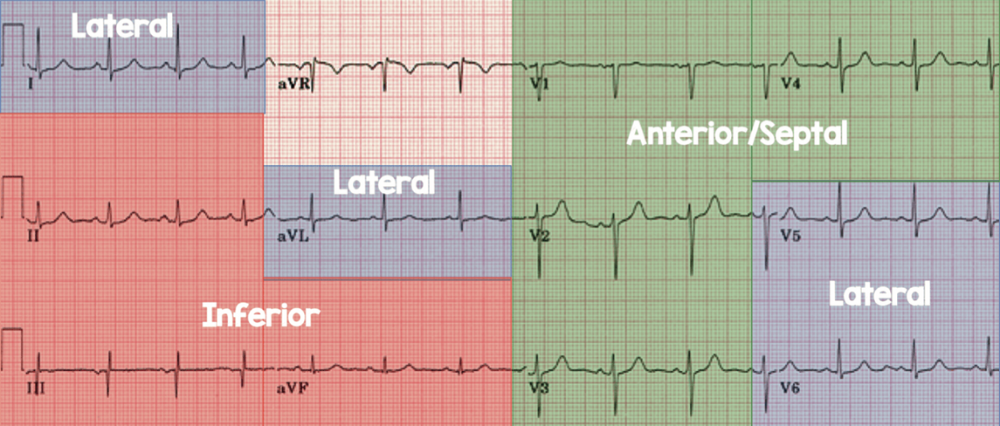
What leads look at what part of the heart?
Each lead represents a different view of the heart. It is important to know this because when there are abnormalities in certain leads you need to refer to the area of the heart which is affected. For example, if the patient has ST elevation in leads II and III, you would hand this over by saying, “the ECG shows inferior ST elevation.”
When we refer to contiguous leads, this means leads of the same view. Leads II, III and aVF are all contiguous leads because they all view the inferior aspect of the heart.
Steps to reading a 12 lead ECG
It is common for student paramedics (in fact, all ambulance clinicians) to become overwhelmed when interpreting the 12 lead ECG. It is therefore important to have structure. By using these 7 simple steps, you will have a structure and be able to interpret the 12 lead ECG without missing anything, whilst not becoming overwhelmed with the amount of information.
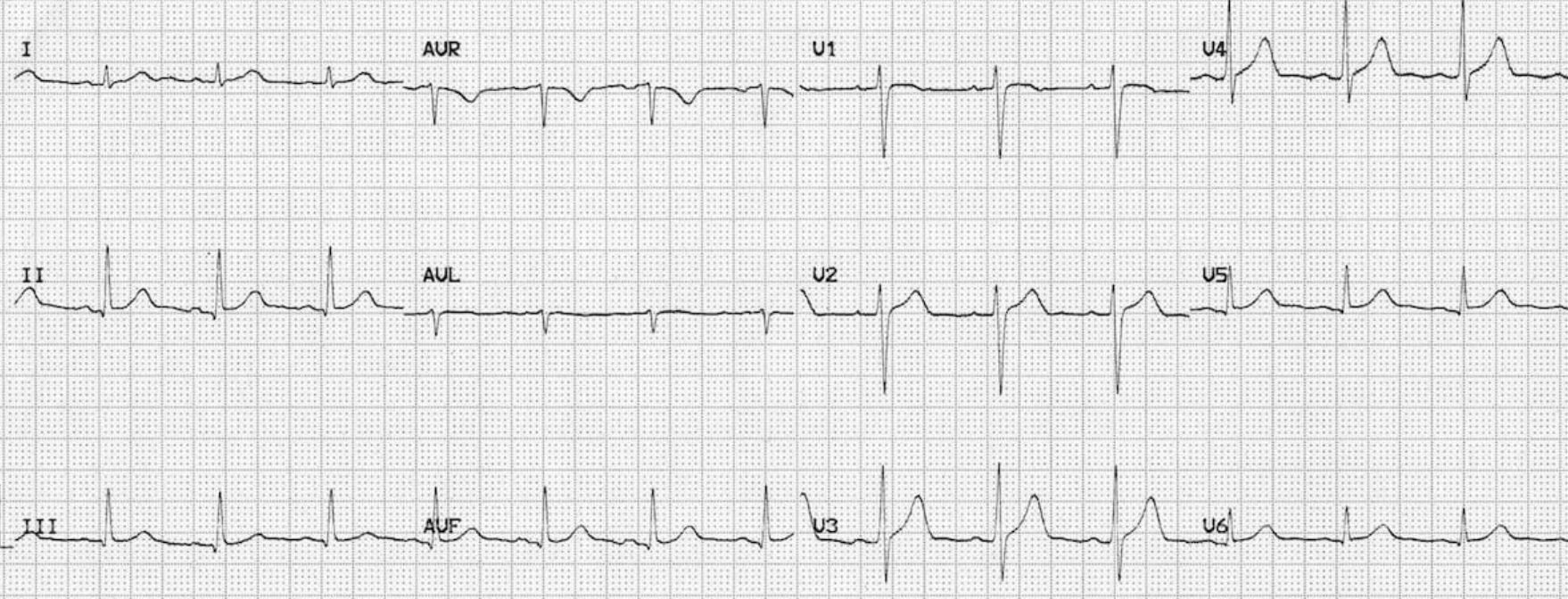
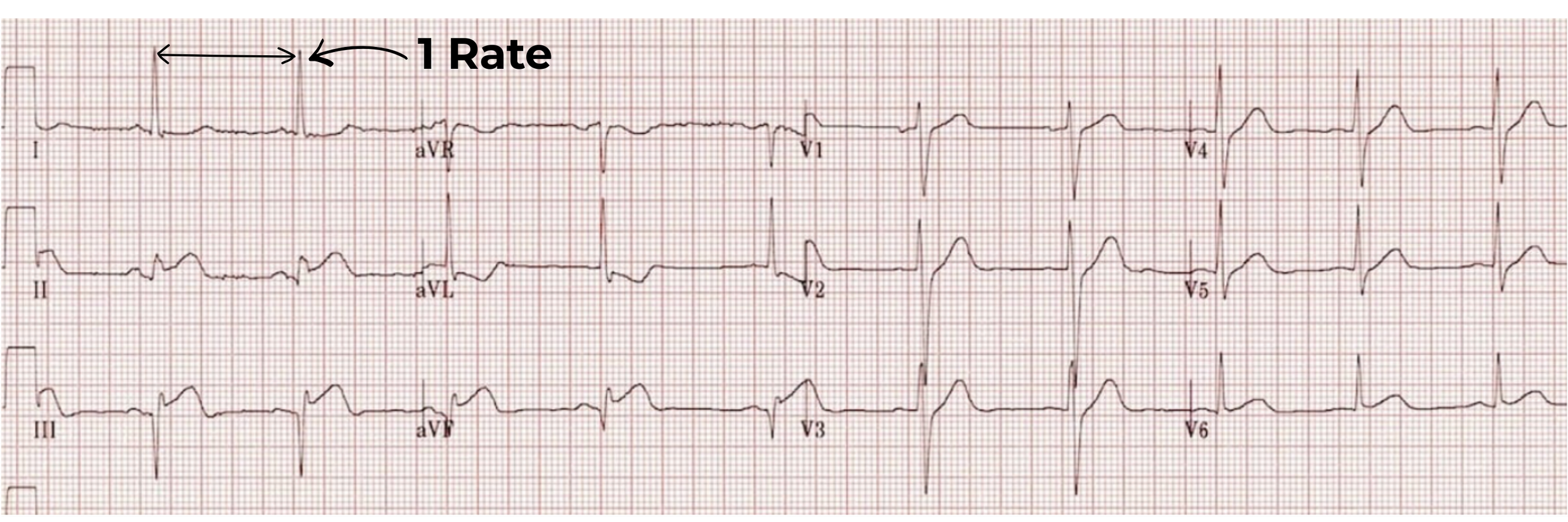
1. Rate
Measure the ventricular rate. You can do this by dividing 300 by the number of large squares in between two QRS complexes. This is because on ECG paper, there are 300 large squares in one minute.
In this example, there are 5 large squares in between the QRS complexes. So, 300/5 = 60, giving us a heart rate of 60bpm.
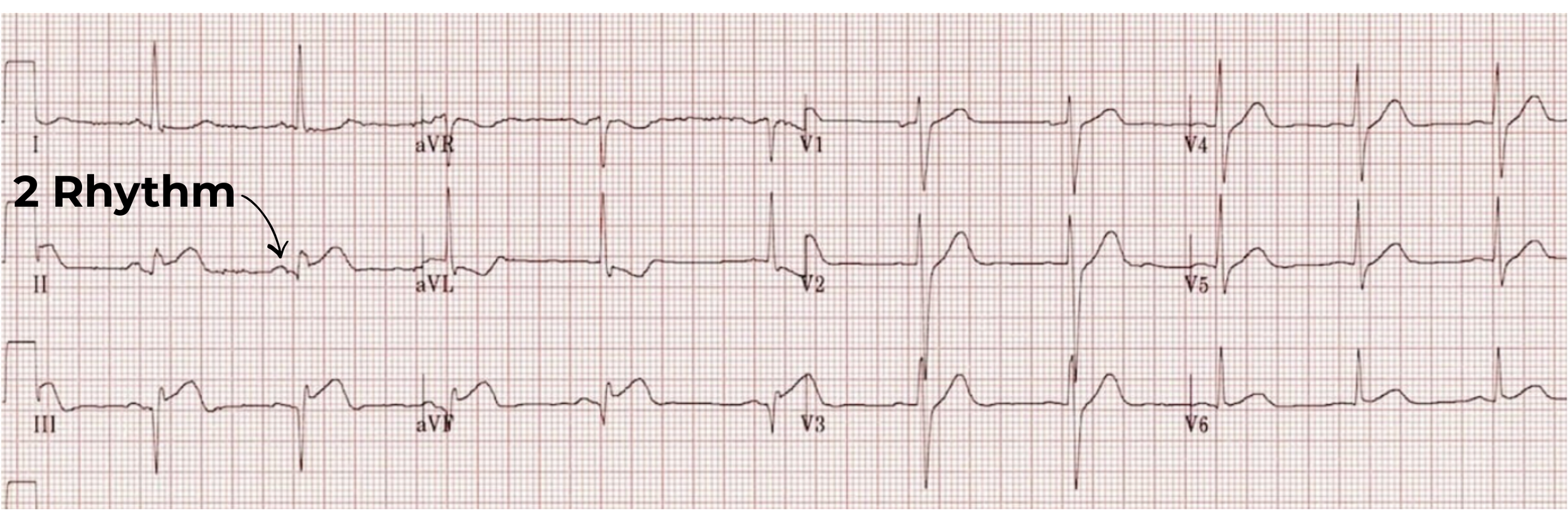
2. Rhythm
Assess the rhythm. This is to see where the impulse originates from.
Always look in lead II when assessing the rhythm. If you have an upright P wave followed by a QRS in each beat, with the P wave being upright in lead I and II, and inverted in lead aVR with a constant PR interval, you know the beat originates from the SA node and is therefore ‘sinus.’
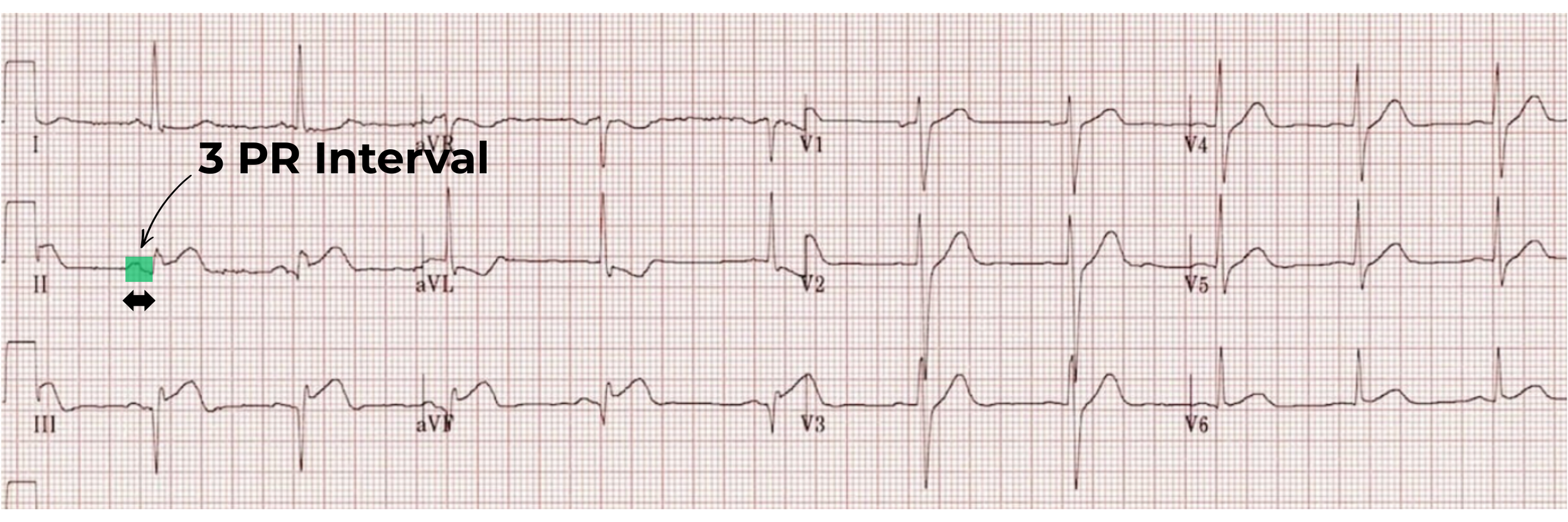
3. PR Interval
The PR interval is from the start of the P wave to the start of the QRS complex. Assess this for AV blocks or accessory pathways.
A normal PR interval is between 0.12s to 0.2s (3-5 small squares).
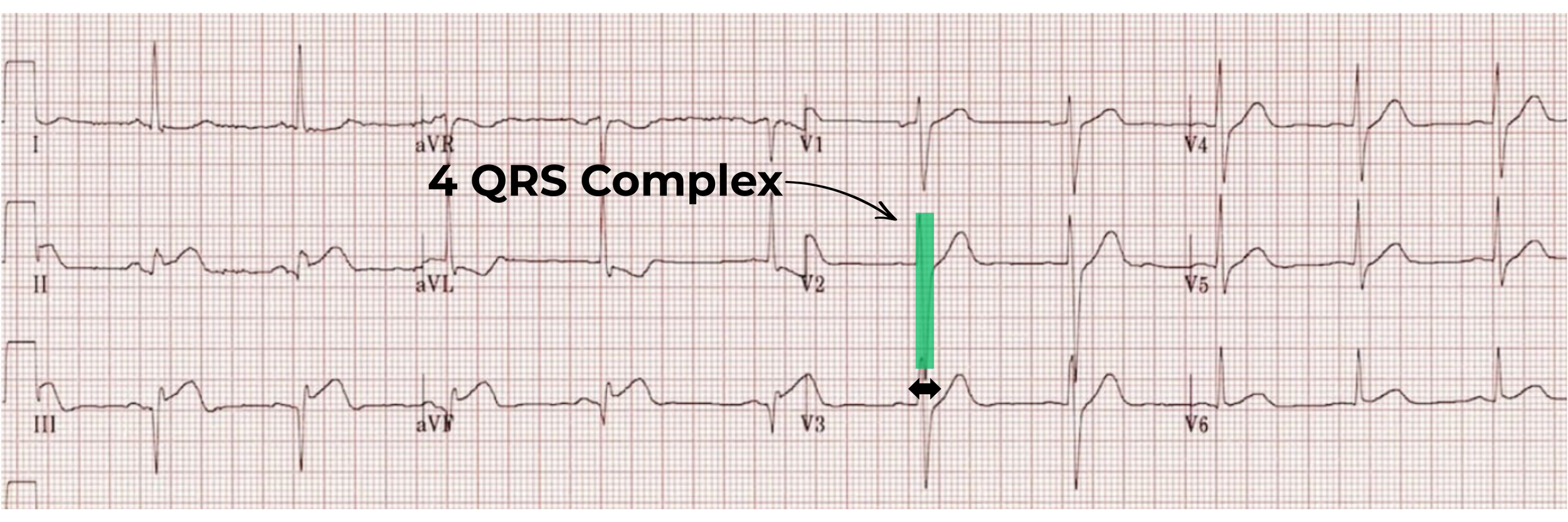
4. QRS Complex
The QRS complex is from the start of the Q wave to the end of the S wave. Assess the width of the QRS complex for conduction delays or abnormal rhythms originating from below the bundle of his.
A normal QRS width is less than 0.12s (3 small squares).
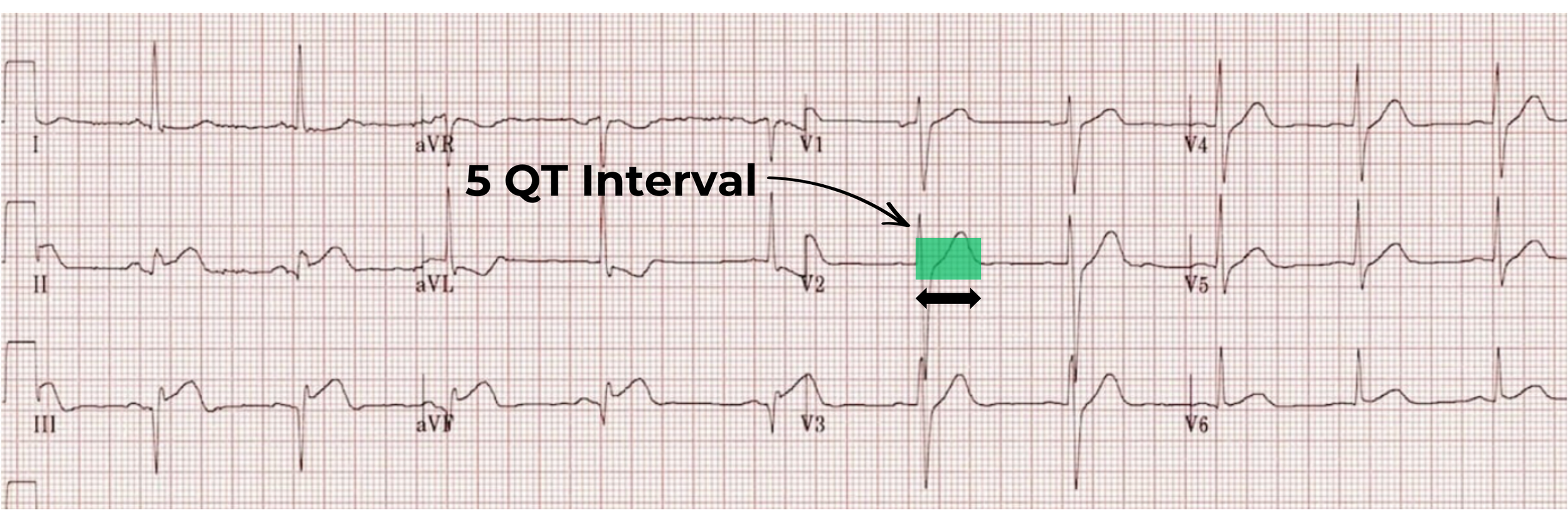
5. QT Interval (QTc)
The QT interval is from the start of the Q wave to the end of the T wave.
QTc is considered prolonged if it exceeds 440 ms in men or 460 ms in women.
A QTc > 500 ms is associated with a significantly increased risk of torsades de pointes.
QTc is considered abnormally short if it is < 350 ms.
As a practical rule of thumb, a normal QT interval is less than half of the preceding RR interval.
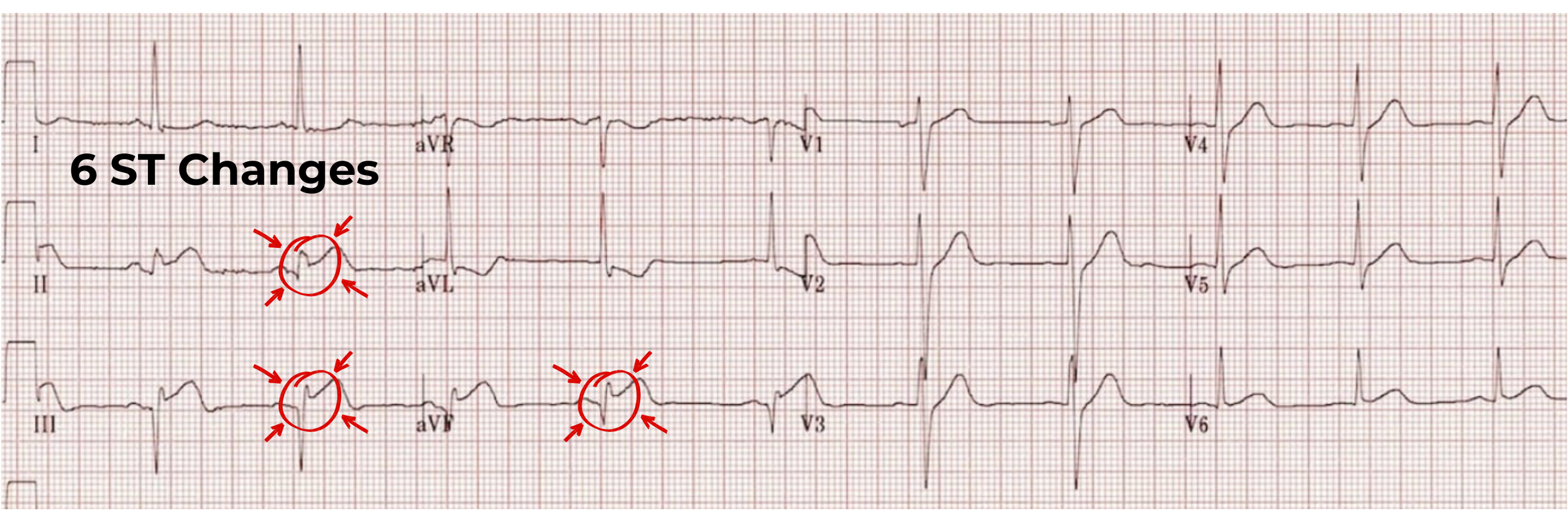
6. ST Changes
The ST segment is area between the end of the QRS complex and the start of the T wave. The ST segment should remain on the isoelectric line.
In this example, you can see the ST segment is above the isoelectric line in leads II, III and aVF. Circle abnormal ST segments on your ECGs.
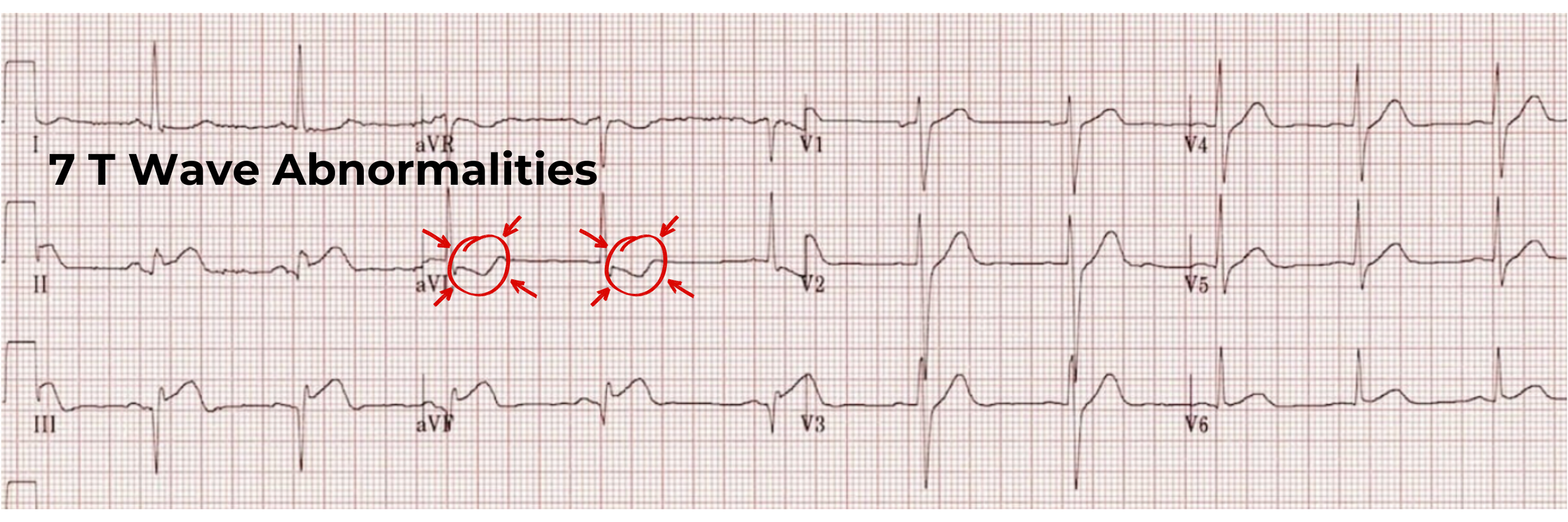
7. T Wave Abnormalities
The T wave represents ventricular repolarisation. Abnormal T waves can be caused by electrolyte changes, myocardial infarction/ischaemia, ventricular strain patterns, pulmonary embolism, and more! Circle any abnormal T waves on your ECGs.
Once you have gone through these seven steps you will have identified any abnormalities and be able to proceed with any treatment and management plans appropriate for the patient.
This page provides a basic introduction to ECG interpretation. To further progress and deepen your 12 lead ECG knowledge, PocketClinician provides many ways to ensure you have all the learning aids available.
PocketClinician supports ongoing ECG development through:
Continue Your ECG Learning
ECG Pocketbook
Structured ECG interpretation guides covering rhythms, abnormalities, and exam-ready explanations.
ECG Video Course
A 28 ECG video course starting at the basics. Giving you a visual and interactive course.
ECG Community
Regular ECG exposure, discussion, and shared learning with other student paramedics and clinicians.
Why 12-Lead ECGs Matter in Pre-Hospital Care
In ambulance practice, 12-lead ECGs are not performed routinely on every patient. They are used selectively when the findings may influence clinical decision-making, urgency, or destination choice.
For student paramedics, the value of the 12-lead lies in:
Early identification of myocardial ischaemia or infarction
Supporting clinical impression in patients with chest pain, dyspnoea, syncope, or collapse
Providing objective information to receiving teams
Guiding urgency of conveyance
A 12-lead ECG does not replace clinical assessment — it supports it.
Key Takeaway for Student Paramedics
A 12-lead ECG is not about spotting one dramatic change — it is about seeing the heart from multiple perspectives and interpreting those findings in clinical context.
When approached calmly and systematically, 12-lead ECGs become one of the most useful tools in pre-hospital care.